University of Chicago researchers are building a 'bionic breast' to restore sense of touch for mastectomy patients
Published in Women
The diagnosis shattered the young mother’s world.
At 36, Heather Tubigan of west suburban Chicago discovered an avocado seed-sized lump in her left breast. It was a malignant tumor. The cancer had already spread to her lymph nodes.
Terrified, the patient almost reflexively asked her surgeon to remove both of her breasts, even though the cancer afflicted only one side.
“I just want to get rid of them both,” Tubigan, now 40, recalled. “I just wanted them out. … When you have cancer, you just want to get rid of it.”
Yet the surgeon urged her to reconsider. While the breast with the tumor had to be removed, the physician explained that there were many benefits to keeping the healthy breast intact — including preserving feeling on one side of the chest, which would be gone on the other side after surgery.
That loss of sensation is often more profound than many breast cancer patients can initially comprehend while grappling with a life-changing illness. From the warmth of a hug to sexual arousal, modern medicine is just beginning to appreciate the various functions of the breast as well as how lack of sensation post-mastectomy can alter the lives, intimacy, sexuality and emotions of breast cancer survivors.
“I was going back and forth for so long. Do I keep it? Or do I not?” Tubigan recounted. “Because just the thought of not having my breast and not being able to feel, that was very, very difficult to me. I couldn’t really understand it. You can’t wrap your head around it, to not have any sensation or any feeling.”
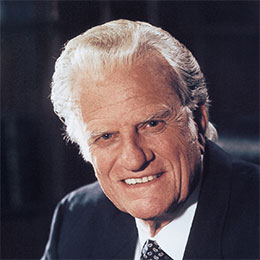
In a groundbreaking project, University of Chicago-led researchers are working to restore that sense of touch for patients who have undergone mastectomy. The team of doctors, neuroscientists and bioengineers is building an implantable device dubbed the “bionic breast,” which will be designed to revive feeling post-mastectomy and reconstruction.
“Our surgical approach to reconstructing breasts after cancer treatment has been focused heavily on the appearance, the form of the breasts, rather than the functions,” said Dr. Stacy Tessler Lindau, principal investigator of the Bionic Breast Project and UChicago Medicine gynecologist. “And we’re trying to change that understanding with our work.”
The first clinical trial to test a key component of the device is expected to start early 2025, Lindau said.
There are more than 4 million breast cancer survivors in the United States, according to the American Cancer Society; more than 100,000 patients undergo mastectomy each year nationwide.
The bionic breast project received a $3.99 million grant from the National Cancer Institute in summer 2023 to begin clinical trials. The implantable device is partly based on the work of University of Chicago neuroscientist Sliman Bensmaia, whose research helped develop prosthetic limbs that restored a realistic sense of touch to patients who were paralyzed or had amputation.
Lindau and Bensmaia partnered for about seven years to work toward applying a similar technology to restore a sense of feeling in the breast post-mastectomy, until Bensmaia’s sudden and unexpected death at age 49 in August 2023.
While breast reconstruction can cosmetically rebuild the look and form of the chest, Lindau said many mastectomy patients still experience a sense of physical and psychological loss akin to that of a person who loses a limb.
“Some women describe the loss of their breasts as … the loss of their identity, the loss of their femininity,” she said. “And it is an existential loss. It calls into question, for some people, their humanity.”
‘Connection with your child’
After much contemplation, Tubigan had a unilateral mastectomy in 2020 and kept her right breast.
She’s grateful her surgeon, Dr. Nora Jaskowiak, surgical director of the UChicago Medicine Breast Center, took the time to counsel her through the decision, weighing the risks and benefits of removing one breast versus both.
The bionic breast project is intriguing to Tubigan: The possibility that an implantable device could one day return a sense of touch to her left side is exciting, she said.
“I’d actually be interested in doing it,” Tubigan said. “To not have that sensation, I’ve learned life without it. But of course, I’d be open to (restoring) it as well.”
Now in remission, Tubigan said having a sense of touch in her remaining breast can be incredibly comforting, particularly when embracing her 9-year-old son Ryker.
“When I hold him on my right, I can really feel him,” Tubigan said. “On my left side, I don’t really feel anything. I only feel pressure, is the best way to explain it. There’s no sensitivity to it.”
Her surgeon stressed that each breast cancer case is different; Jaskowiak said she tries to help patients better understand their options and what the long-term ramifications of different treatment paths might be.
But sense of touch in the breast is one important factor that patients might otherwise overlook.
“We spend tremendous time talking people through it, really having them informed about these choices,” she said. “When you hug someone, if you have a bilateral mastectomy, you’re not going to have that sensation on your chest wall. Or when you hold your grandchild … you’re not going to have that feeling of a child sitting against your chest when your breast is completely numb.”
These lifelong consequences can be hard to take into account as women are making treatment choices in a moment of fear and anxiety, Jaskowiak added.
“There’s all kind of stuff about breast and chest sensation that we just don’t think about,” she said. “But then, it can be lost.”
Throughout her battle with breast cancer, Tubigan and her husband longed to have another child.
“And we didn’t know if cancer took that away from us,” she said.
Prior to undergoing chemotherapy and radiation therapy, she had her eggs harvested to safeguard her fertility. But earlier this year, she and her husband conceived on their own.
“We miraculously got pregnant naturally,” she said.
On Nov. 8, Tubigan gave birth to a girl. Shortly after delivery, she nursed her newborn on her right breast, feeling her daughter suckle and snuggle against her chest during the feeding.
“For me, when breastfeeding, you share this connection with your child. And it’s a beautiful thing,” she said. “It’s not easy. It’s not for everyone. But I think it’s an amazing thing that the human body can do. You can produce a life … but being able to produce food and nutrition for your child, it just shows another sense of love.”
Faith rewarded
For more than 14 years, Lindau has specialized in the field of onco-sexuality, helping cancer patients recover their sexual function during and after treatment.
While she cares for patients with all types of cancer, more than half have breast cancer.
“I came to appreciate how loss of sensation of the breast — and even pain and sometimes itching and other symptoms in the breast — really interferes with sexual function,” she said. “The breast is a very important sexual organ for most women.”
Lindau explained that the nipple-areolar complex has an erection function, a similar physiology to the penis and clitoris. And for many women, if they lose the nipple, they’re not able to have an orgasm; this can be a particularly difficult problem for women who have had double mastectomy.
One day, a patient turned to Lindau and asked, “What are you going to do about this?”
Around the same time, the physician became familiar with the work of Bensmaia, an international expert in the neuroscience of touch, whose lab and research partners at the University of Pittsburgh developed a robotic prosthetic device that restored a realistic sense of touch and allowed the patient’s thoughts to control the prosthetic arm and hand.
A 28-year-old man who was paralyzed used that prosthetic to fist-bump President Barack Obama in 2016, an iconic moment Obama invoked during his farewell address in Chicago in 2017.
“I’ve seen our scientists help a paralyzed man regain his sense of touch,” the president had said, remarking on the wonders he’d witnessed throughout his eight years in office. “So that faith that I placed all those years ago, not far from here, in the power of ordinary Americans to bring about change — that faith has been rewarded in ways I could not have possibly imagined. And I hope your faith has too.”
Bensmaia had explained to the Tribune in 2011 that the usefulness of a prosthetic is limited without tactile feedback. For example, when lacking a sense of touch, patients cannot distinguish between the textures of corduroy and silk, similar objects such as a pen and a pencil, or even the feel difference between a poke compared to a punch.
“People take (their sense of touch) for granted more than vision or hearing,” he had said at the time.
Lindau approached Bensmaia and asked if he thought his work on the prosthetic hand could be translated to the breast.
“And he said, yes, I agree with you that that’s a viable concept,” she recalled. “He was exceptionally excited because, although it’s very meaningful work to be able to restore sensation to a prosthetic hand, the number of people with that kind of an amputation injury who would be eligible for sensory restoration was small.”
In comparison, the number of breast cancer survivors who might benefit from a bionic breast was “orders of magnitude greater,” Lindau said. In August 2023, Lindau and Bensmaia received the multimillion dollar National Cancer Institute funding for the clinical trial.
“And he passed away a few days later,” she said. “I felt an immense sense of loss due to the tragedy. And a double-down commitment to bring the bionic breast project to life.”
Experiments, bold vision
For the first clinical trial, the project will recruit participants who are already planning to undergo a two-stage double mastectomy with breast reconstruction procedure.
When the mastectomy is performed, the breast tissue will be taken out like it normally is; the breast portion of the intercostal nerves, which run along the ribs in the chest and provide sensation to the breast, will also be removed during this process, Lindau said.
To the cut nerves, the reconstructive surgeon will attach small electrodes connected to tiny electrical leads, which look similar to an old-fashioned coil telephone cord but are about as thin as coarse strands of hair; those electrical leads will travel out of the skin under the arm. The mastectomy incision will then be closed and the patient will heal, Lindau said.
About six weeks later, the participant will come into the clinical research center and the project team will connect the leads coming through the skin with an energy source.
“And those experiments will help us identify and answer the question — can we deliver energy to these nerves in a way that restores sensation?” Lindau said. “We’re having participants do that with us using very similar protocols that have been used in people with limb amputation to demonstrate that delivering electricity can indeed restore sensation.”
The patients will report back describing the sensation, intensity, and whether the feeling is natural or painful, to help researchers better design the device; the electrical leads and electrodes would later be removed from those participants during breast reconstruction.
The team will later test the whole “bionic breast” device: This will involve implanting a flexible sensor underneath the patient’s skin that will be able capture the pressure of a hug or the sensation of a gentle touch, Lindau said.
The sensor would take in the mechanical information of touch and transmit it to a processor in the chest that can convert that information into electricity, which would then be delivered to the nerves, Lindau said.
This would all occur “through a closed system that’s implanted in the breast,” Lindau said.
She said this implantable device would be designed to be compatible “with the widest range of procedures” mastectomy patients can elect.
Some patients decide to undergo reconstruction with breast implants; some opt to remain flat with no reconstruction. Others choose to have what’s called flap reconstruction, a procedure that uses tissue from another part of the patient’s body to rebuild the form of the breast.
“So in one case, (the device) might be fully integrated with an implant,” Lindau said. “In another case, it might operate without any implant at all.”
Even with an “ambitious timeline,” Lindau estimated the technology wouldn’t be available to the public for at least five years, and that’s if the trials go as expected.
“But we are working with urgency, recognizing how many women are suffering with loss of sensation after mastectomy,” she added. “And we are working with a big, bold vision.”
‘A need to feel touch’
Breast sensory function is often overlooked by medical practitioners caring for breast cancer patients, Lindau said. But she and her colleagues are trying to change that.
A few years ago, she launched the FEEL Project in collaboration with the Bionic Breast research group, to inform the public about the impact of mastectomy on sensation. That work included interviews with breast cancer survivors and medical providers about loss of feeling after surgery, which were compiled in a video.
These narratives were intended to give patients an idea of what to expect after mastectomy, as well as provide a guide for surgeons to discuss breast sensation with patients.
“You know if you sit on your leg for too long and it falls asleep and finally, when you’re trying to get sensation, it aches a little bit but yet you can’t feel anything? That’s how it felt,” one unilateral mastectomy patient said in the video. “Around the nipple itself? Absolutely nothing. I think one day I pinched as hard as I could. Nothing.”
“You never think about, what does your breast mean for you during sex. It just happens,” another breast cancer survivor commented during the video. “But when you’re going to lose your breast, and you do, then you’re like yeah, that really was important to me.”
A psycho-oncologist explained during the video that loss of breast sensation can be very distressing, but will vary from person to person.
“We all have a need to feel touch, which can be a source of pleasure, as with intimacy, but also a source of comfort, as with a hug,” she said.
One of the patients interviewed was Tubigan, who described the change post-mastectomy.
“It’s just different now,” she said in the video. “Even my son knows, if we’re cuddling and watching a movie, he’ll put his head on my right side versus my left side.”
During the interview, Tubigan also expressed gratitude for her surgeon, Jaskowiak, who removed one breast to help save her life and encouraged her to keep the other one, preserving a sense of feeling on one side, a piece of her identity as a woman and her ability to breastfeed her daughter.
“What helped me get through it was, my surgeon just provided space and really was open to hearing my concerns,” Tubigan said in the video. “And she didn’t see me as a number.”
If she hadn’t gone to Jaskowiak, she wonders if she would have undergone a double mastectomy, losing all feeling in her chest as well as the chance to nurse her new baby.
She named her daughter Nora, after the surgeon.
_____
©2024 Chicago Tribune. Visit chicagotribune.com. Distributed by Tribune Content Agency, LLC.

















Comments