UnitedHealth Group CEO acknowledges frustrations with US health care system
Published in Business News
The UnitedHealth Group leader whose murder in December unleashed a torrent of public frustration and dissatisfaction with the U.S. health care system was pushing for some of the very improvements that critics have been seeking.
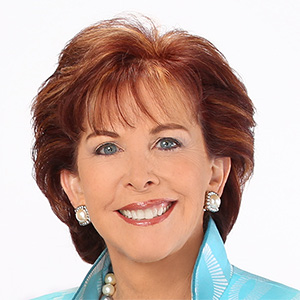
Andrew Witty, CEO of the Eden Prairie, Minnesota-based health care giant, made the comments Thursday during a conference call with investors that he opened by acknowledging condolences many have offered since the fatal ambush of Brian Thompson, 50, of Maple Grove.
Thompson, the chief executive of the UnitedHealthcare health insurance division, was gunned down Dec. 4 while he walked on a public sidewalk in New York City, about to enter a company meeting with stock analysts.
Witty said Thompson worked on improvements to prior authorization rules that are part of a broader system for claims processing that can frustrate patients and health care providers, even as it plays a role in UnitedHealth Group’s vision for how to lower costs and improve quality. The work to improve the prior authorization continues, he added.
The country’s system for health care offers the most advanced clinical care in the world, Witty said, and remains a global destination for patients in part because it’s been tailored to meet individual needs. At the same time, industrywide fixes are needed for handling medical claims, he said, and the experience for consumers suffers from too much confusion and complexity.
“America faces the same fundamental health care dynamic as the rest of the world: The resources available to pay for health care are limited, while demand for health care is unlimited,” he said.
The commentary came as UnitedHealth Group released financial results showing the company beat estimates for fourth quarter earnings by posting a profit of $5.54 billion during the final three months of 2024.
Despite the earnings, the company’s stock price fell 6% Thursday as UnitedHealthcare reported a surprisingly high ratio of medical costs to premium revenue.
“There may be some investors that may be taking a wait-and-see attitude, to see how cost trends unfold over the course of the year,” said John Boylan, an analyst with Edward Jones.
In the aftermath of Thompson’s killing, some took to social media to celebrate accused shooter Luigi Mangione, saying he exacted a measure of justice on a health care system that leaves too many patients feeling powerless, particularly when health insurers deny coverage for care.
Mangione did not have coverage through UnitedHealthcare. Yet the company’s status as the nation’s largest health insurer, and one of the biggest corporations in the U.S. overall, puts it in the middle of questions about the need for systemic change.
Last week, a group representing faith-based shareholders petitioned UnitedHealth Group to develop a report on the human and economic toll stemming from limits and delays to accessing health care paid for by UnitedHealthcare. The company says critics have spread misinformation about its track record denying health insurance claims.
During the conference call Thursday, one stock analyst asked Witty to comment on the sources of dissatisfaction with the U.S. health care system, and how UnitedHealth Group could respond.
Witty said one set of problems involves claims processing, since patients and health care providers get frustrated with the time required for insurers to pay for services. There’s also confusion, he said, about the process that insurers use when asked to pay these bills.
Less than half of 1% of all claims are denied for clinical reasons, Witty said, such as an insurer’s determination that health care providers are recommending unsafe or less-effective treatment options.
Many other claims are held up much earlier in the process because they’re sent to the wrong company or lack information, he said, adding that sometimes patients just don’t have benefits that cover the service.
On prior authorization, Witty said: “We already have advanced plans ... to use standardization and technology to speed up turnaround times for approval of procedures and services for Medicare Advantage patients and to materially reduce the overall number of prior authorizations used for certain MA services.”
Procedure and prescription costs are higher in the U.S. than many other countries, Witty said. Controlling expenses is controversial, since doing so hits revenue for other industry players.
Witty singled out drug manufacturers, asserting that his company’s pharmacy benefit manager — Optum Rx — is helping control drug costs, contrary to the assertion of critics who say the company and other PBMs benefit financially from drug price inflation.
Witty pledged that Optum Rx by 2028 would pass through all rebates it negotiates with drug companies to the governments and employers who hire the business.
“Last year, our PBM passed through more than 98% of the rebate discounts we negotiate with drug companies to our clients,” he said. “While we offer customers 100% pass-through options, a small number have historically elected other models.”
Witty added: “We will continue to encourage all of our clients to fully pass these (rebate) savings directly to patients.”
UnitedHealth Group offers a path forward, the CEO argued, through a concept called “value-based care,” which includes changing the way health care is paid for to promote quality and prevent illness while discouraging waste and inefficiency.
At the same time, he acknowledged that Americans are frustrated by a health care system that’s more difficult to interact with than banks, retailers, streaming services and other sectors of the economy.
UnitedHealth Group continues to invest in technology to close the gap for consumers, the CEO said. But he stressed how fixes in health care aren’t easy.
“The core fact is that price, more than utilization, drives system costs higher,” he said.
UnitedHealth Group is one of the largest companies in the country, with about 400,000 workers overall, including about 19,000 in Minnesota.
At the end of December, about 49.3 million people in the U.S. had coverage from UnitedHealthcare, up slightly from the total at the end of September.
The company also runs Optum, a division for health care services ranging from outpatient medical centers to pharmacy benefits management. It served about 100 million consumers during the fourth quarter.
On Thursday, UnitedHealth Group reported adjusted earnings per share of $6.81, which was 7 cents better than expected among analysts surveyed by LSEG Data and Analytics.
Quarterly revenue of $100.8 billion trailed analyst expectations for sales of $101.7 billion.
The fourth quarter results released Thursday were better than year-ago quarterly earnings of $5.46 billion on $94.4 billion in revenue.
The company this year expects an adjusted profit of about $27.1 billion to $27.7 billion on revenue of $450 billion to $455 billion.
©2025 The Minnesota Star Tribune. Visit at startribune.com. Distributed by Tribune Content Agency, LLC.






Comments