UnitedHealthcare's second largest market is Florida. What does that mean for insurance denials?
Published in Business News
FORT LAUDERDALE, Florida — About 4 million people in Florida are insured by UnitedHealthcare, a company facing backlash after its CEO was shot to death in Manhattan, followed by public outrage over its pattern of coverage denials.
Florida represents UnitedHealthcare’s second largest market after Texas, providing coverage through employee plans, the Affordable Care Act open marketplace and Medicare Advantage plans.
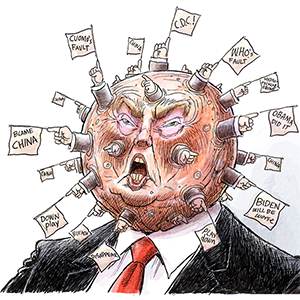
This week, the insurer’s prior authorization and coverage denials in the state drew the same anger and frustration seen nationwide on social media in the wake of the shooting. Florida lawyers, insurance advocates and medical billing experts say being informed about UnitedHealthcare’s practices, making smart choices and fighting back is critical, especially now that the insurer uses sophisticated artificial intelligence (AI) to deny approvals and claims. According to consumer research site, ValuePengiun, UnitedHealthcare denies claims at a rate nearly double the industry average and now faces a barrage of lawsuits, including hundreds in Florida.
“People are paying lots and lots of money for this insurance and then they get screwed over by the company,” said Doug Wolfe, a healthcare attorney and managing partner of Wolfe Pincavage in Miami. “They’re giving all this money to them, and when they need it the most, they deny the claim.”
Of UnitedHealthcare’s Florida members, over 1.2 million seniors hold Medicare Advantage plans. Experts say seniors need to be particularly aware of their rights as they become increasingly more likely to have their claims denied, pay more for premiums and medical visits, and face unexpected costs for care they thought was covered by their health plan.
An October Senate report shows one of the biggest complaints against UnitedHealthcare is that it denies senior Medicare Advantage plan holders approval for rehabilitation or nursing care after hospital stays at far higher rates than other types of care. The report found that UnitedHealthcare authorized home health services instead, which cost the insurer less and require a heftier patient responsibility.
“UnitedHealthcare is a master at using their technology to deny claims that can end up costing the patients more money,” said Wolfe, whose Miami law firm has cases representing thousands of claims against UnitedHealthcare on behalf of hospitals and medical practices throughout Florida.
As an individual, navigating the pre-authorization and payment denial process requires stamina, attention to detail, and often legal representation. Experts say it is usually worth the effort, especially when receiving needed medical care or the reality of medical debt hangs in the balance.
A KFF analysis of privately managed Medicare Advantage plans discovered only about 10% of patients appeal insurance denials, and about one-third of those appeals fail.
“About 50% of the bills we see have mistakes in them, and that has a ripple effect for the policyholder,” said Caitlin Donovan, spokeswoman for The Patient Advocate Foundation, a nonprofit that assists patients with appeals. “If you scrutinize your bill or denial for the mistake, it’s probably there. But most people don’t take the time to look for it or to appeal.”
Donovan said when her foundation investigates, it often finds the insurer is making denials when they shouldn’t be. “It’s not fair that burden is falling on patients, especially as they’re going through medical issues. But pushing back on a denial is probably worth your time.”
How to make an appeal
Donovan said patients denied prior authorization or payment should dig through the insurer’s denial letter to find instructions for the appeal process.
“Your denial will include details as to why they are making this decision, so you have to counter that with the facts that support your argument,” she said.
The Patient Advocate Foundation has sample appeals letters on its website.
When planning an appeal, document every step of the process, advises Russel Lazega, a Dania Beach insurance claims lawyer.
“Don’t treat an internal appeal to the insurer informally,” Lazega said. “A lot of people call and talk to the insurance company and don’t document it.”
Documentation should include emails from the insurer to the patient or from the patient to a doctor or hospital.
“Gather a direct response to their denial from your doctor and add your additional medical records to it,” Lazega said.
Sometimes, that documentation is enough to win an appeal.
If unsuccessful, the next step is an external appeal to a company hired by the insurer. “It’s important to have your documentation in the file. Any documentation pertaining to your appeal won’t be looked at unless it’s already in the file. Adding it later is hard, so don’t give the insurance company that technical advantage,” Lazega said.
The final step is federal court.
Lazega said people in life-or-death medical situations tend to go this route. The patient pays legal fees, not the insurance company.
“UnitedHealthcare approves and pays about 90% of medical claims upon submission,” UnitedHealthcare said in a statement provided to the Sun Sentinel. “Importantly, of those that require further review, around one-half of one percent are due to medical or clinical reasons. Highly inaccurate and grossly misleading information has been circulated about our company’s treatment of insurance claims.
“We do not use AI to make adverse coverage determinations. Coverage decisions are based on CMS coverage criteria and the terms of the member’s plan.”
It’s not just patients fighting back
Hospitals are fighting back against insurer rejections, too. Most have their own artificial intelligence to scan denials for mistakes. They hire companies like Health Business Solutions in Davie to appeal fees that UnitedHealthcare refuses to pay when it deems a procedure or treatment unnecessary.
“I have doctors and nurses on my staff who take the medical record, review it and write why the patient needed the treatment they received and why the insurer should pay,” said Ray Berry, CEO of Health Business Solutions. “However, the insurance company has the final say, unless you take them to court.”
Berry said that two out of every 10 hospital claims are denied by insurers. His firm works to lower those denial rates and increase the percentage of successful appeals.
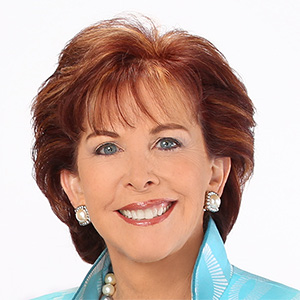
Doctors say they are fighting denials, too. Dr. Georgiy Brusovanik, a Miami spine surgeon, says he tries to help patients obtain coverage, but also finds himself fighting for his fees from the insurers. “The problem is they just don’t pay me,” he said of UnitedHealthcare. “They usually get you on a technicality.”
Donovan says policyholders should know that the process begins well before the appeals stage. It starts with open enrollment and knowing the coverage details and co-pays for the plan you choose, she said.
“It’s so important that you’re making sure when you’re picking your plan, especially when you are older, that you have good benefits and are actually covered for what you think you are,” she said. “Most people don’t take the time to do that.”
©2024 South Florida Sun Sentinel. Visit at sun-sentinel.com. Distributed by Tribune Content Agency, LLC.






Comments