Mayo Clinic Q&A: What is macular degeneration?
Published in Health & Fitness
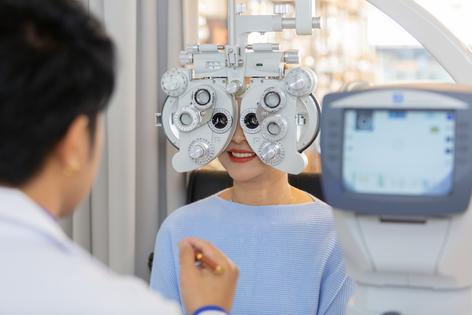
DEAR MAYO CLINIC: I recently celebrated my 50th birthday and had an eye exam. The ophthalmologist recommended that I get screened for macular degeneration. I was surprised because nobody in my family has had any eye issues, and I am not having trouble with my vision. I know there are many health screenings I need as I age, but is this a new recommendation or simply because I'm getting older?
ANSWER: Happy birthday and welcome to your 50s. As you noted, screening recommendations often are based on age, including those for your eyes. Age-related macular degeneration is the No. 1 cause of vision loss for adults over 50. It may run in families but not always, so a routine screening is recommended for most people as they get older.
Age-related macular degeneration is an aging-related change that affects the retina, particularly the macula. The macula is a portion of the retina with specialized cells that allow you your sharpest vision. Your retina consists of layers of neural tissue that line the back part of the eye and send information from the eyes to the brain.
Just like a baseball diamond infield is where most of the action happens during a game, most of the important vision tasks are done by the cells in the macula. This includes things like reading, recognizing faces and viewing road signs.
Degeneration means a deterioration of vision. There are two types of macular degeneration. Nonexudative age-related macular degeneration, also called dry macular degeneration, may take a long time and proceed slowly, but it can cause severe central vision loss over time. Exudative age-related macular degeneration, also called wet macular degeneration, can cause permanent and rapid central vision loss.
Dry macular degeneration develops first, and a physician who specializes in eye care — an optometrist or an ophthalmologist — can detect it during a dilated eye examination. This likely is the type of screening your eye doctor recommended at your exam.
Dry macular degeneration is the most common form of age-related macular degeneration and can be associated with gradual blurriness of the central vision or occasional waviness of straight lines, such as light poles or the edge of a doorway. If the retina is compared to a large field, dry macular degeneration is like getting pebbles, dry patches, or large potholes, or experiencing loss of all the grass.
Dry macular degeneration may be asymmetric, and one eye can be more affected than the other. Over time, vision worsens and affects the ability to perform everyday tasks. Having dry macular degeneration doesn’t mean you will lose all your sight. Vision loss involves your central field, and you lose your ability to read and recognize faces.
Wet age-related macular degeneration, the exudative form of the disease, can cause sudden blurriness to complete loss of central vision. Wet or exudative refers to the growth of abnormal blood vessels called neovascularization. This can leak serum and blood under and into the retina. This leads to slippery localized conditions, presenting as distortion and small spots, to a complete washout, presenting as a total central loss.
The exact cause of macular degeneration is unknown, but there are things you can do to decrease your risk of developing the condition. Anyone over 50, especially those with a parent or sibling with macular degeneration, should follow these tips:
You can’t reverse damage caused by macular degeneration, but treatments can slow the progression and preserve existing vision when started early. During your 50s and beyond, continue to visit your optometrist or ophthalmologist for routine exams, as well as for any sudden central vision loss. — Michael Scott, M.D., Ophthalmology, Mayo Clinic Health System, La Crosse, Wisconsin
(Mayo Clinic Q & A is an educational resource and doesn’t replace regular medical care. This Mayo Clinic Q&A represents inquiries this healthcare expert has received from patients. For more information, visit www.mayoclinic.org.)
©2024 Mayo Foundation for Medical Education and Research. All Rights Reserved. Distributed by Tribune Content Agency, LLC.






Comments