White House rule would expand access to cost-free birth control
Published in News & Features
WASHINGTON — The Biden administration on Monday proposed making over-the-counter contraception available at no cost and with fewer administrative hurdles.
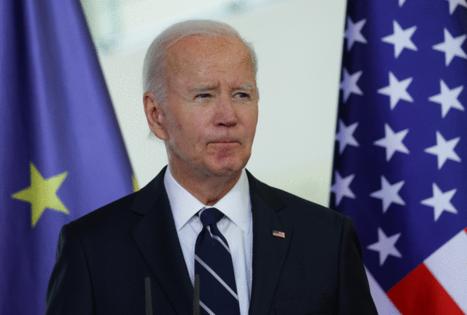
“Today, my Administration is taking a major step to expand contraception coverage under the Affordable Care Act. This new action would help ensure that millions of women with private health insurance can access the no-cost contraception they need,” President Joe Biden said in statement.
The proposed rule — issued jointly by the departments of Health and Human Services, Labor and Treasury — seeks to require insurance plans to cover OTC contraceptives at no cost and without a prescription for individuals with commercial insurance plans. Health plans would also be required to tell beneficiaries about the policy and would expand their required coverage of preventive services for prescribed contraceptives without cost sharing.
Under the 2010 health care law, most private insurance plans must cover birth control without cost sharing. Currently patients can get coverage without cost sharing for over-the-counter contraceptives, including oral contraceptives, spermicide and condoms with a prescription, such as female condoms, or through their provider in a health facility, or for long-acting services like an IUD, which is an intrauterine birth control device.
If finalized, the rule would require plans to make all available OTC contraceptive products available through in-network pharmacies. A senior administration official said logistics would be clarified in the final version of the rule.
“This new proposed rule will build on our Administration’s work to protect reproductive freedom by providing millions of women with more options for the affordable contraception they need and deserve,” Vice President Kamala Harris said in a statement. “That includes coverage for no-cost over-the-counter contraception without a prescription for the first time in our nation’s history.”
Jennifer Klein, assistant to the president and director of the White House Gender Policy Council, called the proposed change the “most significant expansion of contraception coverage under the Affordable Care Act in more than a decade” in a call with reporters.
The proposed change comes on the heels of the rollout of the first available OTC contraceptive pill earlier this year. The Food and Drug Administration approved the Opill, the progestin-only birth control pill made by HRA Pharma, in July 2023. Progestin is a synthetic hormone used in birth control.
The pill became available in March 2024 for $19.99 for a one-month supply or $49.99 for three months, but advocates have called for bringing down the price and requiring insurance coverage of the drug.
HHS, Labor and Treasury initially put out a request for information on covering OTC preventative services, including a daily contraceptive pill, in October 2023.
The Biden administration said that rule would also reduce barriers for prescription-based contraceptives for plans that use medical management to only cover certain types of drugs.
The same senior administration official said the rule seeks to make the exceptions process more transparent for contraception by modifying how types of birth control are categorized. Currently, insurers must cover at least one product per category type, but the rule would change this requirement to one product per therapeutic equivalent.
This process, the official said, would also make it easier for a patient’s provider to still ensure the patient is able to receive a contraceptive outside of what is covered under the plan, if an exception is required, while still being no cost to the patient.
It’s unclear when the rule could be finalized and if or when it would take effect given the upcoming change in administrations.
The senior administration official said the rule would take effect during plan years after the rule is finalized, which could be in 2025.
HHS also issued clarifying guidance, in partnership with Treasury and Labor, that insurers must accept industry-standard coding for standard preventive care services including colonoscopies and pre-exposure prophylaxis, which is used to reduce the risk of contracting HIV.
The administration has previously received complaints from patients and providers after insurers charged patients for recommended preventive services.
HHS Secretary Xavier Becerra said the guidance will reduce barriers to accessing these preventive services and ensure individuals can receive them without cost-sharing.
___
©2024 CQ-Roll Call, Inc., All Rights Reserved. Visit cqrollcall.com. Distributed by Tribune Content Agency, LLC.



Comments